
Fungal infections of the feet begin in areas between the toes. Subsequently, the infection can spread to the feet and nail beds. The disease is caused by dermatophyte, mold or yeast fungi. According to statistics, in our country about 20% of people have fungus on their feet. The severity of the disease depends on the type of infection, but in any case the disease must be cured, since peeling, severe itching, inflammation and unpleasant odor of the feet cause severe discomfort. We will tell you how to get rid of foot fungus.
What does foot fungus look like?
A fungal infection causes inflammation of the skin where the fungal infection is located. The main types of dermatomycosis of the legs are:
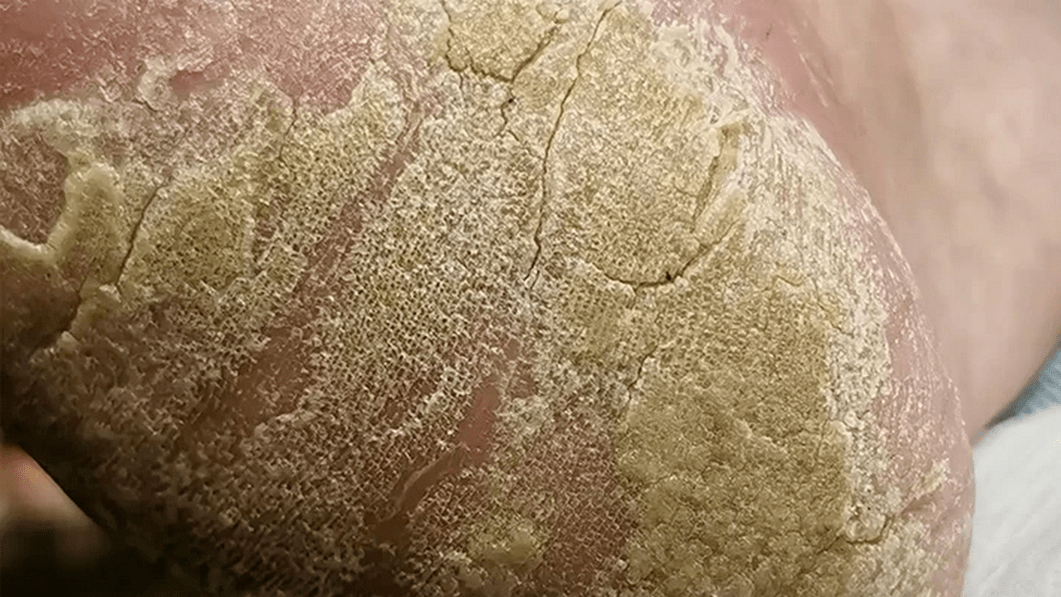
- Fungus of the sole of the foot is squamous, in which the affected area turns red, peels, and cracks appear on the skin. The patient often does not experience any discomfort, which contributes to the widespread spread of this type of disease.
- Dyshidrotic foot fungus is localized on the arch of the feet, which are not in contact with the floor surface. At the sites of infection, small blisters form, which spread to the inner and outer parts of the foot, open, forming erosions and diaper rash on the surface of the skin. The process is accompanied by a feeling of itching and burning. After opening of the vesicles (bubbles), the disease passes into the squamous form.
- A fungus on the skin of the feet that affects the interdigital space is called the intertriginous form of the disease and is its most common type. It appears in the form of cracks, the edges of which are covered with a white rim of exfoliating epidermis. As a rule, this form has a long-term chronic course and is difficult to treat.
- Fungus on the shin or ankle appears as round spots of pink or red color, covered with skin scales. As the infection progresses, the foci of inflammation grow, the process is accompanied by severe itching.
Onychomycosis
This disease is a type of foot fungus characterized by fungal infection of the nail. You can become infected in public showers, saunas, baths, and swimming pools. Scales containing a pathogenic microorganism are quite easily separated from the nail plate and can remain on floors, carpets, bedding, and unpainted benches. High humidity allows them not only to survive, but also promotes active reproduction, and therefore the risk of infection increases significantly.
At the initial stage, the infection reaches the epidermis of the feet, causing severe itching. In order to ease the discomfort, a person begins to comb the infected area, but this only worsens the situation. Areas of skin affected by the fungus become covered with small scratches and cracks, microorganisms begin to spread, penetrate under the nail plate, and then begin to multiply uncontrollably.
Severe illnesses such as diabetes or HIV, poor circulation, or injury to the nail greatly increase the risk of infection.
Onychomychosis is divided into 3 types:

- Normotrophic. With this type of onychomycosis, a change in the color of the nail from normal to yellow-brown is observed. The natural shine, shape of the nail and its thickness remain unchanged.
- Hypertrophic. A final change in the color of the nail occurs, its shine disappears, its shape changes, thickening develops and partial destruction begins.
- Onycholytic. The color of the affected nail changes to brown, it becomes thinner and begins to break. Its gradual separation from the bed begins. Uneven layers may appear on the exposed part of the nail bed.
Treatment of this type of fungus on the palms and soles with topical medications is ineffective due to the fact that the fungal spores are located under the nail. Before starting treatment, the nail should be removed. This is done with the help of keratolytic drugs, and patches are also used. In some cases, it is possible to remove the nail mechanically: parts of the nail that have died are cut off with a nail file or nippers. It is important to remember that all instruments used must be sterile.
The combined use of mechanical removal and keratolytic patches is the most effective way to remove diseased nails. As for keratolytic agents, you can use a ready-made kit with a broad-spectrum antifungal drug. It contains a special ointment, files for scraping the nail, and a patch. After the nail plate has been removed, you should start taking systemic antifungals: an antifungal drug for systemic use, an oral antifungal agent.

Symptoms
Depending on the form of the disease and the location of the inflammation, the infection is accompanied by different symptoms with a number of the following general signs:
- peeling of the skin;
- slight or severe redness of the skin at the site of the lesion;
- itching;
- burning sensation;
- blistering rashes or cracks in the skin.
Blisters between toes
The main symptom of athlete's foot, caused by Candida fungus, is the appearance of blisters between the toes, usually between the fourth toe and the little toe. The course of the disease is accompanied by swelling of the skin adjacent to the fingers, pronounced areas of redness with small blisters on their surface. The source of inflammation is surrounded by a rim of exfoliated epidermis.

Dyhydratic form
Vesicular fungus, or, as it is also called, dyshydratic mycosis, is the rarest type of disease. Its main manifestation is numerous vesicles united in conglomerates. Vesicles are bubbles filled with pus or nutrient fluid from the inside. When the fluid begins to become cloudy, the vesicles burst, leaving ulcers in their place. They begin to merge into one line, forming pronounced scars on the skin. This occurs due to drying and peeling of the skin layers.
About 70% of infections with vesicular fungus are accompanied by allergic rashes. A variety of bacteria and viruses begin to penetrate the ulcers. As a result, the disease becomes mixed, and identifying the original pathogen becomes more difficult. Therefore, you should consult a doctor as soon as the primary symptoms appear: he can quickly identify the type of foot fungus and begin therapy.

Moreover, this should be done immediately. First of all, before using antimycotic drugs, the acute process should be eliminated. It is better to entrust this task to a specialist: he can carefully puncture the vesicles, treat the remaining ulcers with two percent boric acid and apply a brilliant green solution or methylene blue.
Treatment of advanced disease involves the use of corticosteroid ointments. After eliminating the inflammatory process, it is recommended to use topical antimycotic agents. This will suppress the pathogen. We continue to consider the names and types of foot fungi.
First signs
Disease of the skin of the legs is always accompanied by a number of general symptoms, the appearance of which indicates infection of the skin with spores of harmful microorganisms. You should seek help from a dermatologist in the following cases:
- the appearance of cracks or blisters on the skin in the folds of the feet or between the toes;
- coarsening and significant thickening of the skin of the feet;
- redness of areas of the skin, their peeling;
- burning or itching sensation.

Duration of treatment
Combined infection of the skin and nail plate requires rehabilitation therapy for one to three months. These terms are considered standard for the most effective pharmaceutical products from a medical point of view.

Pregnancy requires a charming visit to the doctor to choose a way to get rid of mycodine infection. Potent medications and therapies that require the use of similar medications are prescribed only under the supervision of a physician in compliance with strict dosages. Many antibacterial tablets that effectively destroy fungus can cause noticeable harm to the fetus. Therefore, whenever possible, during pregnancy, patients are recommended to be treated using traditional medicine recipes. Many of them allow you to cope with the disease, but provided that the disease has not reached a complex stage. Only classical medicine can help cope with the advanced form.
Modern medications allow you to completely restore your legs to health within two weeks, provided that signs of infection were detected in time.
Causes
Infection occurs for a number of reasons after direct or indirect contact of the patient with the carrier of the infection or his personal belongings, household items. Risk factors for contracting tinea pedis include:
- disorders of the leg circulation and related diseases (varicose veins);
- weakened general or local immunity;
- failure to comply with hygiene rules;
- weakening of the body's defense systems after taking antibiotics;
- increased sweating of the skin of the feet;
- presence of minor damage to the skin (abrasions, scratches).
Treatment methods

In most cases, it is possible to completely get rid of a disease detected in time in a maximum of a month. This is a very important point in treatment, since itching, tissue damage and other manifestations disappear, the patient sometimes stops treatment, believing that the disease has been defeated. But remnants of the infection can easily trigger a relapse.
Treatment procedures should be stopped only after the doctor’s permission and after passing the necessary tests. This is especially true for advanced forms of the disease. The fungus is firmly "fixed" in the body and sometimes it can take at least six months to get rid of it. But the external manifestation of fungus on the feet in the form of various damage to the skin or nail disappears much earlier, creating the illusion of health. By stopping therapy in this case, the patient is almost guaranteed to provoke a relapse.
Treatment of feet for mycoid infection is carried out comprehensively. To get rid of the disease, local antifungal drugs and tablets are used to eliminate the infectious agent that has penetrated inside the body. To get rid of itching, pain, brittle nails and accelerate tissue regeneration, certain medications may be prescribed. It is not recommended to combine them independently with the main therapeutic group, so as not to provoke an allergic reaction or poisoning of the body due to the simultaneous use of incompatible drugs.
Cure foot fungus at an early stage is quite simple. Usually, two weeks of therapy is sufficient to eliminate the symptoms of mycoid infection.
Types of mycoses
Only a dermatologist can accurately determine the type of fungus by visual examination, the data of which is clarified using laboratory tests. Depending on the causative agent of the fungal infection (yeast, mold, fungi of the genus Trichophyton or Candida) on the skin of the feet, there are several main types of the disease, which include:
- candidiasis of the feet;
- athlete's foot;
- trichophytosis (or rumbicosis) of the feet;
- onychomycosis (nail fungus).

Prevention
Simple preventive measures will significantly reduce the likelihood of infection. You should use only personal belongings, and treat your nails with sterile instruments. When visiting public places, such as baths, saunas, swimming pools, beaches, you should use your own shoes. By the way, try to choose it so that it is comfortable and allows your feet to breathe. You should worry about prevention in advance so that you don’t have to deal with various types of foot fungus later.
How to treat
Treatment of skin fungus on the legs is a long-term complex therapy, in severe cases including the use of systemic oral agents. For minor lesions, the emphasis is on local therapy using antibacterial and antiseptic agents. In acute forms of the disease, warm baths are prescribed to relieve inflammation and remove dead skin cells. In some cases, it is necessary to treat the patient’s shoes and clothing with special compounds to avoid relapses.
System Tools
Systemic oral agents are prescribed in cases of ineffectiveness of local drugs and in severe advanced forms of the disease. A course of oral antifungal drugs is indicated for fungal infections of the deep layers of the skin; they help not only treat the acute stage, but also prevent the disease from becoming chronic. The dosage regimen, course duration and dosage are selected by the attending physician.
Doctors recognize antifungal drugs for systemic use as the best means for systemic treatment of foot fungus. They have an active fungicidal (destroying) and funginistic (suppressing the proliferation of bacteria) effect; their active components can accumulate in the upper layers of the epidermis, nails and hair. Before taking it, be sure to read the instructions for use, since these products have contraindications.
Local remedies
Therapy with topical drugs includes not only the use of antifungal creams and ointments, but also the use of special sprays, aerosols and lotions. The form of the drug is recommended by a dermatologist, depending on the type of causative agent of the infection, the severity of the lesion on the skin of the legs, the stage of the disease and the individual characteristics of the patient’s body. The duration of treatment with a local drug can range from 2 weeks to 3 months.
For foot fungus and other forms of mycoses of the skin of the legs, an aerosol, a suspension for application to the skin, or a solution for topical use can be prescribed. The products are either applied directly to the skin damaged by the fungus, or wet swabs soaked in a medicinal solution are applied. All necessary recommendations for use can be obtained from your doctor.
Antifungal ointments
When treating foot skin fungus, in most cases an antifungal ointment is prescribed, for example a cream with the active ingredient terbinafine hydrochloride or its analogues. Apply the drug in the form of an ointment or cream to the dry skin of the heels or other areas of localization of inflammation, previously carefully cleaned of dead epidermal cells and any other plaque. For different types of disease, the duration of treatment can range from 2-3 weeks to 2-3 months.
Experts consider broad-spectrum ointments to be effective means for combating foot fungus of various forms and stages. The active components of the drug locally fight fungal infection, suppressing the reproduction of its pathogen. The ointment is applied two to three times a day to washed, affected skin for several weeks or months, depending on the degree of damage to the skin.
Folk remedies
The use of folk remedies is possible only with the consent of the attending physician. The main products for baths, compresses and applications against fungus on the skin of the feet are vinegar, propolis, baking soda, decoctions of medicinal plants, and laundry soap. The following procedures are practiced:
- Baths with a solution of soda and salt. For 3 liters of water at a temperature of 36-40°C, use 3 tbsp. l. salt and 3 tbsp. l soda. The duration of the procedure is 10-15 minutes; after the bath, rinse your feet under running warm water. Used for acute forms of fungus for 7-10 days, twice a day.
- Lotions with herbal decoction. To prepare a decoction, mix dried oak bark, calendula flowers, and verbena leaves in equal proportions. To prepare the decoction 3 tbsp. l. pour a glass of boiling water over the mixture and keep on low heat for 10-15 minutes. Make a compress with the resulting decoction three times a day for 20-30 minutes.

Erased form
Mycosis of the erased form is almost invisible, its symptoms are minimal. These include: mild itching, burning, flour-like peeling, microcracks located in the interdigital areas. If you do not contact a specialist when the first signs of the disease appear, the pathology can develop into the form of onychomycosis, which is much more difficult to treat. In this case, the peeled nail will grow back from one month to six.
Mycosis of the erased form is treated with local preparations: ointments, creams, foams. They allow you to create a layer on the foot that will protect against infection by other infections. It is not recommended to wash your feet for 24 hours after applying this drug.
Only in extreme cases can systemic therapy be prescribed. The problem is that such drugs are toxic and negatively affect some internal organs, such as the liver. Accordingly, if there is an effect from the use of local remedies, then it is better not to take pills.
Routes of infection
Fungal spores remain viable in the environment for a long time, so it is easy to become infected with the disease in the most unexpected places. But the most favorable conditions for their development are warmth and high humidity. Due to this, people visiting the following are at risk:
- swimming pools;
- baths;
- saunas;
- fitness centers;
- beaches.
Fungus can appear on any things located there, even if regular disinfection is carried out. Therefore, in such places you should avoid common objects and be sure to take replacement shoes with you.
Military personnel are at risk. Most often, soldiers in the army wear uncomfortable shoes that do not allow air to pass through. Because of this, the feet sweat, microtraumas appear, into which the fungus penetrates.
There are two types of infection. The first is the direct path through direct contact with the infectious agent while communicating with a sick person, caring for an animal, or walking barefoot on the ground and sand. The second - the indirect route leads to infection through objects belonging to infected people or pets.
Preventive measures

Preventing a disease is always easier and safer for health than treating it, even using the most gentle method. In the case of a fungal infection, prevention is one of the mandatory norms of life, since it is very easy to become infected. Therefore, to reduce the risk of contracting the disease, it is recommended to follow a few simple rules:
- try to eat healthy and eat as healthy as possible;
- do not use other people’s things and personal hygiene products;
- use basic protective equipment in public places, such as replacement shoes and hygienic antibacterial agents;
- wash your feet and change your socks regularly;
- lead a healthy lifestyle;
- Take regular baths to improve foot health;
- periodically disinfect shoes.
Prevention of fungal infection is important not only to prevent it, but also if the disease does occur. In this situation, compliance with sanitary and hygienic standards helps speed up healing and prevent infection of others with the fungus.
















